Case from: Andrew R. Kolodziej, MD, Michael B. Mikolaj, MD, Steve Leung, MD, Vincent L. Sorrell, MD
Institutes:Gill Heart Institute, University of Kentucky, Lexington, KY
Clinical history: 49-year-old gentleman diagnosed with T3aN0M1 metastatic renal cell carcinoma in September 2010, underwent a right-sided nephrectomy the same month. He presented to our emergency department with complaints of constant chest pain, which waxes and wanes in intensity and sharp in characteristic. This was first described as occurring the night prior to his ED visit. The pain was located in the sub-sternal area with radiation to his left side and back. Nitroglycerin provided in the ED somewhat improved patient’s pain.
ECG on presentation showed evidence of anterolateral ST segment elevations with concomitant reciprocal changes in the inferior leads, thus the cardiac catheterization laboratory was activated.
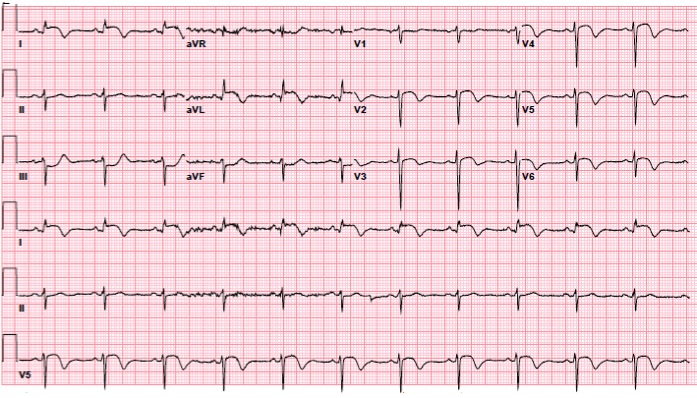
Figure 1. Normal sinus rhythm with left anterior fascicular block and ST segment elevations with T-wave inversion in anterolateral leads and ST depressions in inferior leads.
While waiting for catheterization lab staff arrival, further history revealed that his chest pain began about six weeks prior to this presentation. He was seen at an outside hospital for the same symptoms and underwent emergent coronary angiography. The outside records showed anterolateral STEMI and cardiac catheterization report revealed no obstructive disease. Given this additional history, coronary angiography was aborted as the presentation became more consistent with acute pericarditis. Subsequent troponin was within normal limits, and acute pericarditis regimen with ibuprofen and colchicine was initiated. Since his ECG findings were not classic for acute pericarditis, a cardiac MRI was obtained to exclude myocarditis or renal cell metastasis.
CMR Findings: Utilizing a 1.5T Siemens Aera MRI scanner, imaging sequences included cine with SSFP, T2 weighted dark blood imaging and first pass perfusion at rest as well as late gadolinium enhancement

Figure 2. T2 turbo spin echo of two chamber view showing a large 50 x 30mm, distal anterior wall, T2 enhanced transmural mass extending into the apex. Large bilateral pulmonary nodules involving the pleura.

Figure 3. Two chamber view of a late gadolinium enhancement image showing a large, heterogeneously enhancing mass with central necrosis in mid to distal anterior wall extending into the apex.
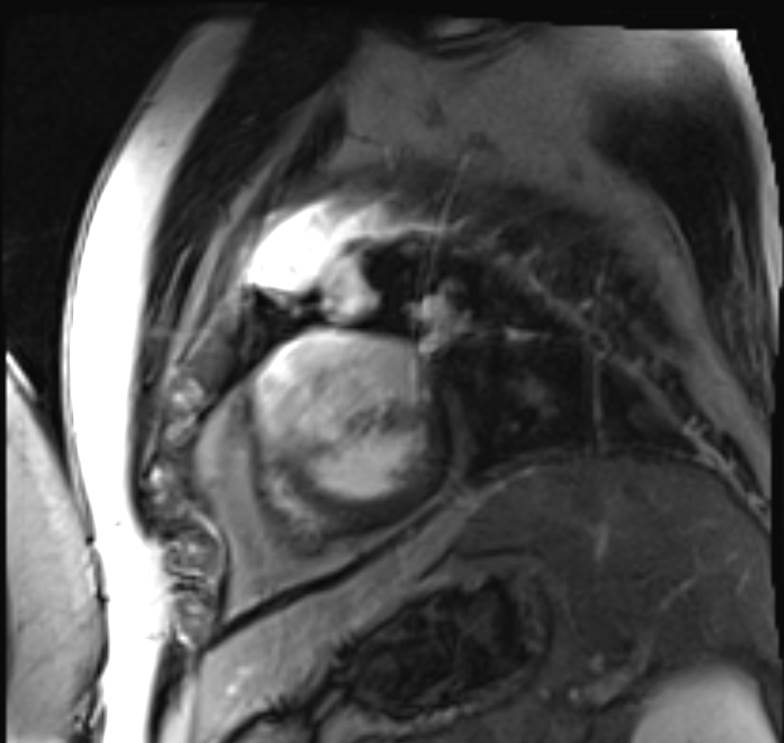
Figure 4. Short axis view of late gadolinium enhancement image showing a large, heterogeneously enhancing mass involving the anterior, septal and lateral walls. Multiple pulmonary nodules as described.
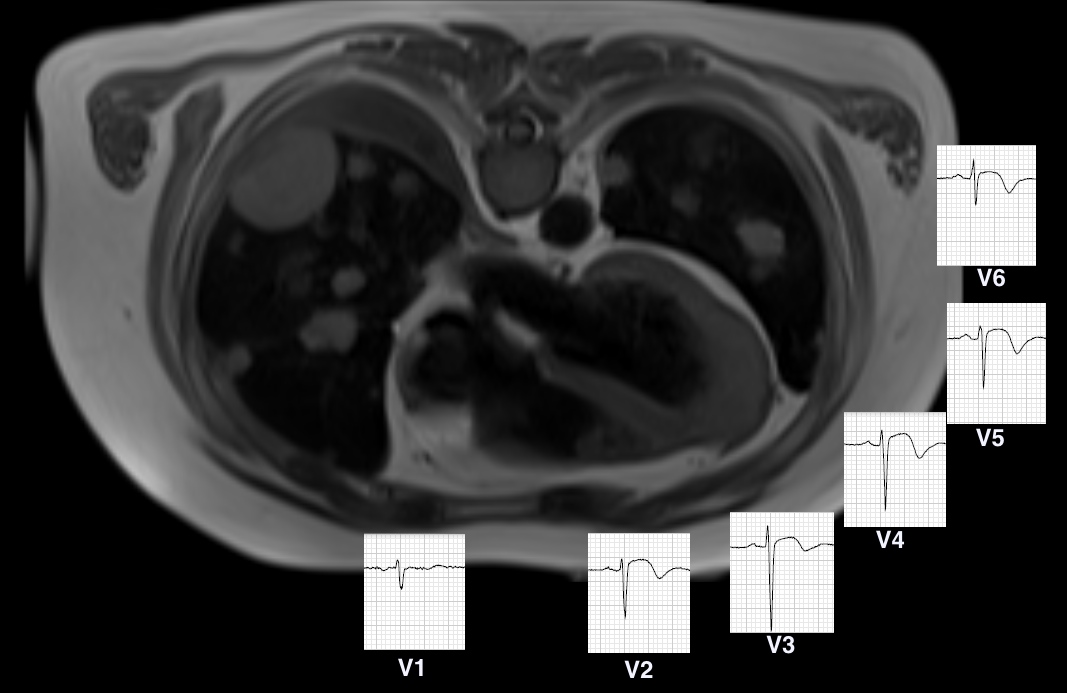
Figure 5. Axial HASTE image showing apical and distal lateral involvement of the myocardium with the mass as well as juxtaposed precordial ECG leads representing ST-segment changes as they relate to the mass.
Movie 1. Cine of 4 projections; two chamber (top left), distal short axis (top right), four chamber (bottom left) and three chamber (bottom right) showing mid to distal anterior wall and distal septal segments (apical short axis view) akinesis
Movie 2. Two chamber first pass perfusion showing a transmural mass with central necrosis in the mid to distal anterior wall.
Movie 3. Distal short axis first pass perfusion showing a transmural mass with central necrosis.
Movie 4. Selective coronary angiography of the left coronary system in LAO-Cranial projection obtained at the outside hospital showing a vascular blush in the distal lateral wall. Otherwise, no obstructive coronary disease.
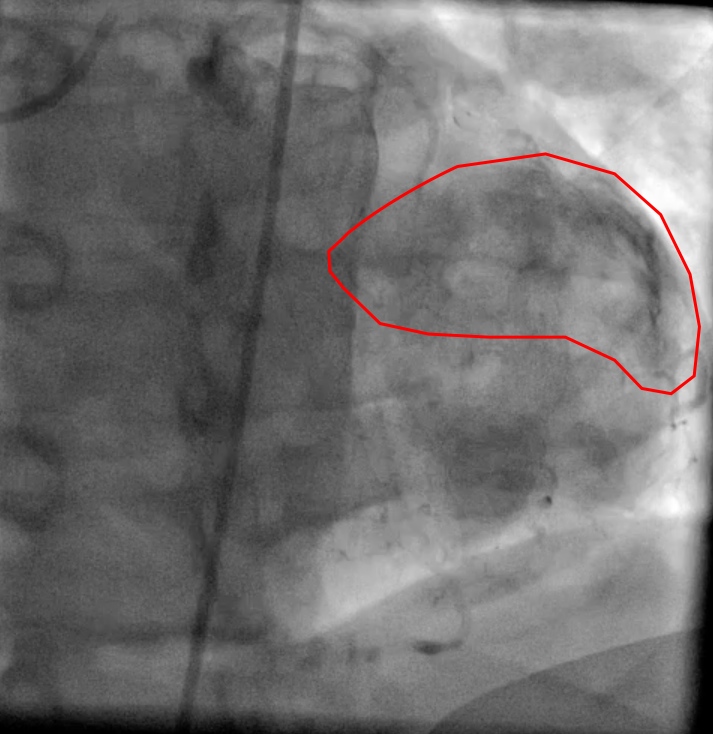
Figure 6. Still image of Movie 4, representing vascular blush (outline)
Conclusion: After realization of the diagnosis by CMR for patient’s chest pain, both colchicine and Ibuprofen were stopped and he was discharged home with plan towards palliative care.
Perspective: Myocardial tumors are more commonly of metastatic origin. The most common neoplasms that metastasize to the heart are lung, stomach, breast and esophageal cancer, as well as those of malignant melanoma and lymphoma. They are 20 to 40 times more common compared to primary cardiac tumors with the majority involving the pericardium and only 5.3 to 10.6% of lung cancer patients experiencing myocardial involvement. The metastatic extension follows several pathways such as direct extension, in addition to venous extension and hematogenous spread, both of which renal call carcinoma utilizes.1
Myocardial metastasis from neoplastic disease is often present with non-specific clinical features and is very difficult to diagnose. ECG abnormalities are commonly seen with tumor invasion of the heart. However, most of these ECG changes are not specific for myocardial involvement and can occur in patients with only pericardial involvement.2 As early as 1944, ST-segment elevation has been reported in cases of tumor invasion of the heart.3 It corresponds to sensitivity of 77% and specificity of 86%.4 The causes of ST-segment elevation in myocardial metastasis are not completely understood. It has been postulated that the inflammatory reactions surrounding metastasis and potassium ion release from necrotic tissue and adjacent myocardium as well as distension of the adjacent myocardial fibers are potential causes.5,6 Others have suggested other possible explanations, including myocardial injury caused by pressure, physicochemical action or by the interference of the blood supply by the invasion of myocardium and intrinsic vascularity of the tumor.3
References:
1. Rathi VK. Cardiac and Paracardiac Masses: Handbook of Cardiovascular Magnetic Resonance Imaging. Editors: Pohost GM, Nayak KS. 2006: Chapter 16, p299-327.
2. Abe S, et al. Myocardial Metastasis from Primary Lung Cancer: Myocardial Infarction-like ECG Changes and Pathologic Findings. Jpn J Med 1991; 30: 213-8.
3. Rosenbaum FF, Johnston FD, Alzamora W. Persistent displacement of the ST segment in a case of metastatic tumor of the heart. Am Heart J 1944;27:667–675.
4. Lestuzzi C. et al. Sensitivity and specificity of electrocardiographic ST-T changes as markers of neoplastic myocardial infiltration. Echocardiographic colleration. Chest 1989;95:980-985
5. Hanfling SM. Metastatic cancer to the heart: review of the literature and report of 127 cases. Circulation 1960; 22-474-83
6. Hartman RB, Clark PI, Schulman P: Pronounced and pro- longed ST segment elevation. A pathognomonic sign of tumor invasion of the heart. Arch Intern Med 1982 142: 1917-1919.
COTW handling editor: Karima Addetia, MD







