Case from: Lilia M. Sierra-Galan1, Ricardo García-Buen-Abad2, Julio César Sauza-Sosa1
Institution: 1Cardiovascular and 2Imaging Divisions, American British Cowdray
Medical Center, Mexico City, Mexico.
Clinical history:
A 28-year-old female at 9.2 weeks of her first pregnancy came to the emergency department for dyspnoea of 3 days duration, NYHA grade 3/4. It was accompanied by pleuritc chest pain in the right hemithorax. She referred having an obstetric ultrasound from a different Institution the day before, which reported a “minimal” placental abruption for which she was currently on aspirin and progesterone, with no vaginal discharge reported. Her pregnancy had been uncomplicated; she referred that her previous obstetric ultrasound was reported as normal. She had history of smoking with a tabaquic index of 5. At her arrival to the ER she had tachypnea (26 RPM) with a heart rate of 93 BPM, the rest of her physical examination was unremarkable: no pleuro-pulmonary syndrome could be established, the gravid abdomen had no pathologic findings, and signs for deep vein thrombosis were negative. Laboratory tests for coagulation revealed a D-Dimer of 3,125 ng/ml, fibrinogen of 684 mg/dl, INR in 0.96, PT of 10.8 seconds, APTT of 25 seconds; other tests performed (including complete blood count, cardiac enzimes, electrolytes and blood chemistry) were within normal limits.
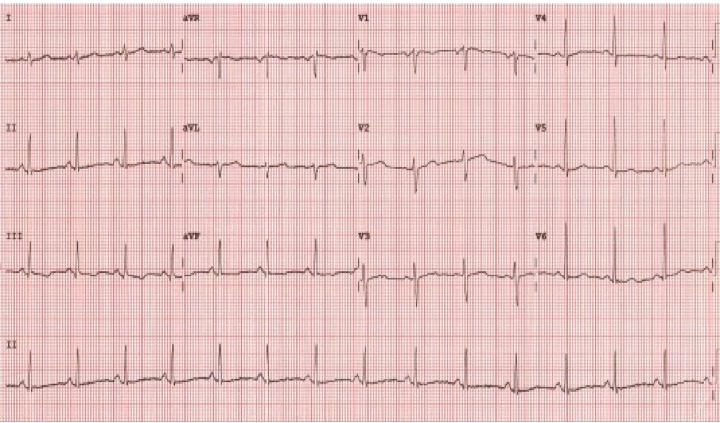
Figure 1.EKG that shows normal sinus rhythm, S1Q3T3pattern and diffuse repolarization abnormalities.
Her attending physician ordered an obstetric ultrasound (US), which showed a gravid uterus with a healthy embryo of 9.4 weeks of gestational age with a fundal retroplacental haematoma of less than 10% and the cervix was closed.
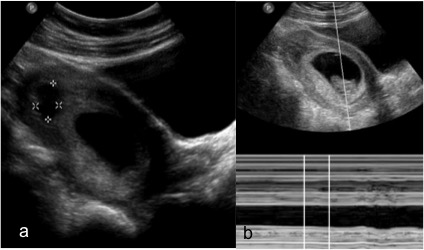
Figure 2.Obstetric ultrasound. (a) US image that shows a fundic placental hypoechoic area of 18 x 12 mm, suggesting a small retroplacental haematoma. (b) US image that depicts the embryo heart rate within normal rages (140 bpm). No active bleeding was detected during exploration and the cervix was closed.
The clinical suspicion at that moment was for pulmonary embolism (PE).
Following the recommended algorithm for maternal imaging in suspected PE1,2, a chest X-ray was first
taken, showing only a mild generalized non-specific lung insterstitial prominence.
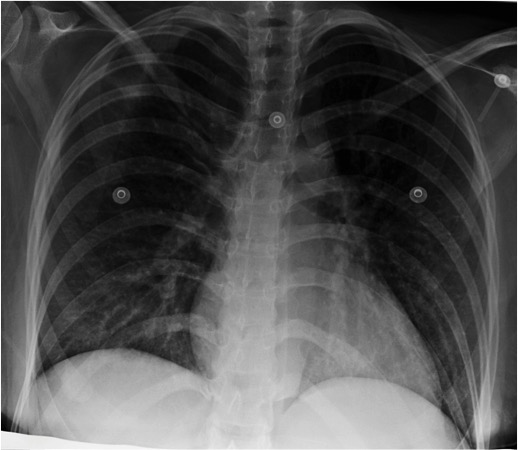
Figure 3.Chest X-Ray, PA projection. Mild non-specific pulmonary interstitial pattern was depicted. There were no opacities suggestives of lung infarction.
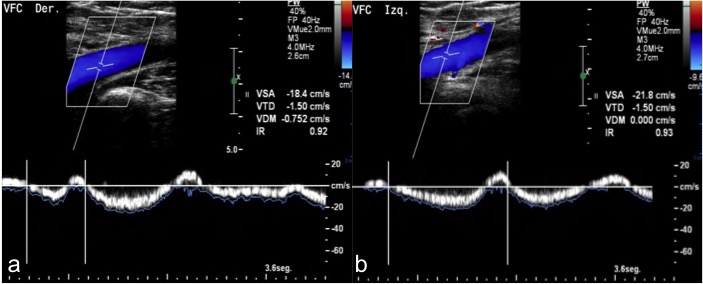
Figure 4.Long-axis color spectral Doppler of the right (a) and left (b) common femoral veins that shows normal phasicity with normal color filling. The profound and superficial vein (greater and small saphenous veins) systems in both extremities where compressible throughout the exploration.
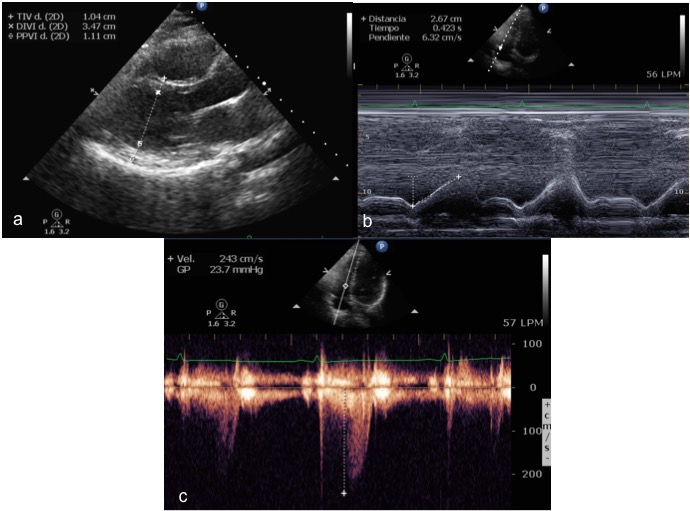
Figure 5.Transthoracic echocardiogram.(a)Parasternal long axis view that shows normal left ventricular inner diameters and wall thickness. (b) M-mode that shows TAPSE of 26 mm. (c) TR velocity of 243 cm/sec consistent with physiological regurgitation and no pulmonary hypertension.

Movie 1.Transthoracic echocardiogram.(left) short axis view that shows normal left ventricular regional wall motion. (middle) apical 4-chambers view that shows normal left and right ventricular global and regional systolic function. (right) apical 4-chambers view with color doppler that shows no significant valvular regurgitations.
We then faced the conundrum of which imaging method would best aid in the diagnosis and do the less harm possible to the embryo. According to the current ACOG guidelines for diagnostic imaging during pregnancy, when PE is suspected, computed tomographic angiography (CTA) and ventilation-perfusion scanning (VPS) are the only imaging methods considered for its diagnosis, without mentioning any special considerations related to the time of pregnancy. To exclude DVT, compression ultrasonography is emphasized, and only if there is doubt for iliac vein thrombosis, MRI is recommended3.
CTA is considered by many the best imaging option for PE during pregnancy, with a better discriminatory power vs. VPS to exclude PE (CTA has sensitivity of 86% vs. VPS of 39%; CTA has specificity of 94% vs. VPS of 97%) and a lower embryonic/fetal radiation dose4,5. However some factors, especially those concerning the first trimester, need to be considered: first, even when diagnostic procedures are below the 5 rad accorded limit for teratogenic effects, stochastic i.e. carcinogenic effects cannot be ruled out; second, the use of contrast agents with iodine derivatives has been linked with neonatal hypothyroidism6.
Given this factors, we decided in consensus with imaging department, ER and her attending physician to evaluate the patient with unenhanced CMR, since it would allow us to assess both the central and first order of pulmonary artery branches and the right ventricular function6,7 without the risk of ionizing radiation or paramagnetic contrast media. We performed an unenhanced CMR with SSFP cine sequences for functional analysis and tissue characterization was done with T1 and T2-STIR sequences of the heart and the lungs.
CMR findings
Movie 2:SSFP Cine images in short axis view (left) andlong axis 4 chambers view (right), which showsnormal left and right ventricular systolic function. No pericardial or pleural effusions were seen.
Movie 3:SSFP Cine images in coronal views (left)and axial views (right), which shows a mobile mass with heterogeneous signal intensity and irregular surface inside the right pulmonary artery extending into the upper and mid right branches, which partially obstructs the flow into the vessel and suggests a recent thrombus.
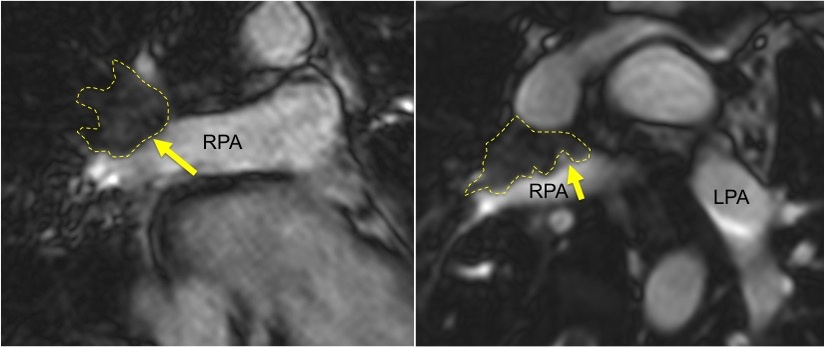
Figure 6:SSFP still image of the coronal view (left) and axial view (right), which shows an irregular mass (arrow and dashed lines) inside the right pulmonary artery extending into the upper and mid right branches, which partially obstructs the flow into the vessel and suggest a recent thrombus.RPA:right pulmonary artery,LPA:left pulmonary artery.
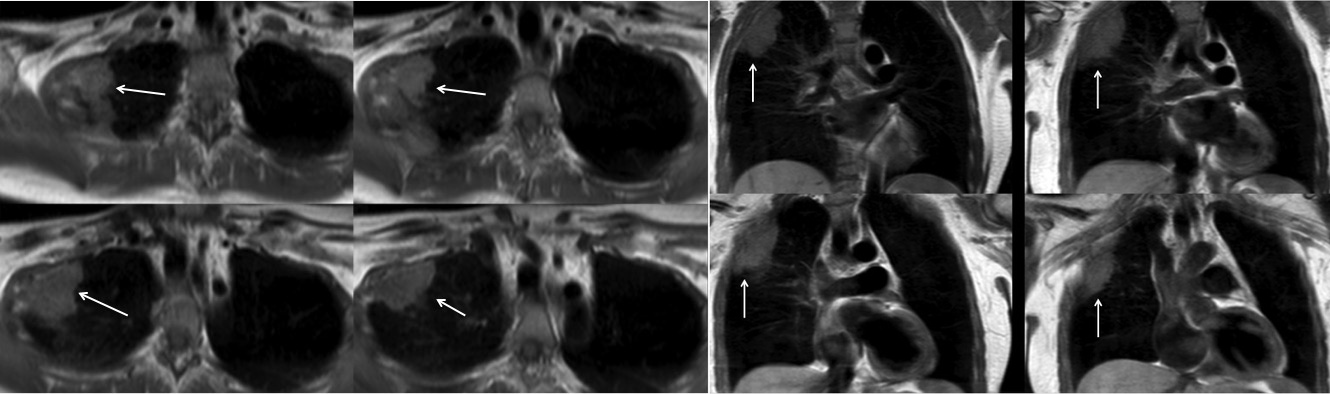
Figure 7:TSE T1-W sequence inaxial images of the upper thorax (left) andcoronal images (right) that shows a triangular mass with heterogeneous signal intensity of irregular surface in the upper anterior segment of the right lung, which corresponds to a pulmonary infarction (arrow).
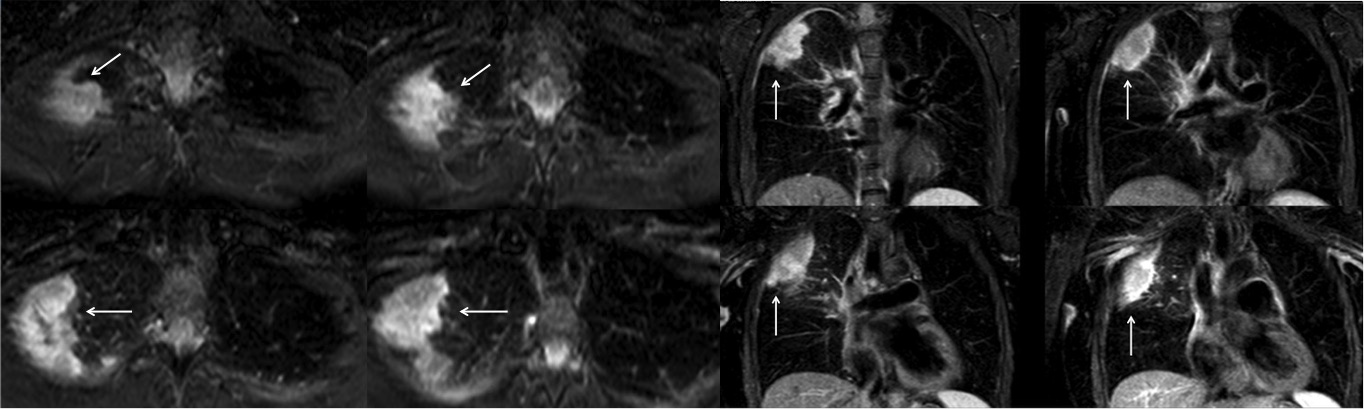
Figure 8:TSE T2-W STIR sequence inaxial imagesof the upper thorax (left) andcoronal images (right) that shows a triangular mass with heterogeneous signal intensity mainly of high signal intensity and of irregular surface in the upper anterior segment of the right lung, which corresponds to a pulmonary infarction and pulmonary edema next to the infarcted area (arrow).
The CMR sequences used in this patient (SSFP cine and T1, T2-STIR) were able to demonstrate the components of the disease, those were shown in detail and the diagnosis was established as PE with associated pulmonary infarction. The patient was then started in enoxaparin 60 mg every 12 hours without complications. A follow up obstetric ultrasound showed a minor reduction in the retroplacental clot and a normal course pregnancy. The patient showed clinical improvement and was discharged on her third day of hospitalization to be followed up by her attending physician. The patient completed her pregnancy uneventfully and delivered a healthy baby.
Conclusions
When PE is suspected during the first trimester of pregnancy, unenhanced CMR combined with compression ultrasonography may be an effective alternative to CTA for its diagnosis. If both tests give negative results for PE and DVT, and clinical suspicion remains high, CTA would still be required to confirm or exclude PE. Unenhanced CMR protocol for suspected PE during early pregnancy is a very good and safer option compared to other imaging techniques using ionizing radiation and that necessarily require the use of iodine contrast media or radioactive isotopes; further evaluation is needed to validate CMR for clinical routine use in this setting.
Perspective
To our knowledge, this is the first case reported of this characteristics: a case of PE during the first trimester of pregnancy diagnosed by unenhanced CMR. Even though there were no contraindications for CTA, as discussed previously, at our Institution, patient safety is first, hence we consider of vital importance to avoid as much as possible any potential risks related to radiation dose during pregnancy, as well as the use of substances that could pass through the hemato-placental barrier, particularly during the first trimester when organogenesis is taking place. Regarding the possible thyroid affection at birth after intravenous iodine derivatives in utero, two major studies concluded that there is no effect on thyroid function, however, in both studies no patient had the contrast media administered during the first trimester of pregnancy, thus we cannot assure with certainty that there are no adverse effects in neonates exposed below 12 weeks of gestational age8. CMR can diagnose central PE without ionizing radiation and contrast media, but its utility is still in dispute. The PIOPED III study investigated the performance of MR angiography (MRA) and MR venography in PE, in this study 93% of patients had proximal PE, the authors found a sensitivity of 92% and specificity 96% when both techniques were combined. Technically inadequate images were found in 52% of cases that limits its diagnostic accuracy, therefore the authors recommend the use of MRI for PE only on centers that routinely do it9. The IRM-EP study evaluated the role of unenhanced-MRI for PE, where 46% of patients had proximal PE, the authors used SSFP with and without ECG-gating, perfusion and MRA sequences, and showed sensitivity for proximal PE close to the one seen at the PIOPED III study (97.7-100%) that diminished with distal PE (segmental of 68-91.7% and subsegmental of 21.4-33.3%). The rate for inadequate images was 32%. They concluded that MRI cannot yet be used as a standalone test for PE, but if combined with compression ultrasound, a negative test could rule out PE7. In a more recent study Kalb et al, combined EKG/respiratory gating MRA with VIBE and non-contrast SSFP, which resulted in sensitivity of 84% and specificity of 99-100%. SSFP alone resulted in a sensitivity of 64% and specificity of 100%10.
The use of MRI for PE during pregnancy is controversial. MRI of 1.5 Tesla is considered safe, but gadolinium is an FDA class C agent. Mudge et al. tested the capability of MRI for diagnosing PE without contrast media using unenhanced SSFP and found 69% sensitivity per vessel and 82% per patient vs. positive CTA2,11,12.
CMR in this setting also helps in identifying signs of pulmonary hypertension and pulmonary infarctions. Since alveolar hemorrhage is present in areas of pulmonary infarction, a hyperintense signal in a wedge-shaped pleura-based consolidation on T1-W images will help differentiate this entity from other causes of pulmonary consolidations, mainly pneumonia13.
A specific CMR protocol for central PE during early pregnancy could be designed to be used as a safer diagnostic imaging modality in this clinical scenario.
References:
1. Pahade JK, Litmanovich D, Pedrosa I, Romero J, Bankier AA, Boiselle PM: Imaging Pregnant Patients with Suspected Pulmonary Embolism: What the Radiologist Needs to Know. Radiographics 2009; 29:639–654.
2. Patel SJ, Reede DL, Katz DS, et al: Imaging the pregnant patient for nonobstetric conditions: algorithms and radiation dose considerations. Radiographics 2007;27:1705–1722.
3. ACOG: Thromboembolism in Pregnancy, Practice Bulletin. Clinical Management Guidelines for Obstetrician-Gynecologists 2011; 118:718-729.
4. Hayashino Y, Goto M, Noguchi Y, Fukui T: Ventilation-perfusion scanning and helical CT in suspected pulmonary embolism: meta-analysis of diagnostic performance. Radiology 2005;234:740-8.
5. Winer-Muram HT, Boone JM, Brown HL, Jennings SG, Mabie WC, Lombardo GT: Pulmonary embolism in pregnant patients: fetal radiation dose with helical CT. Radiology 2002; 224:487-92.
6. ACOG: Guidelines for Diagnostic Imaging During Pregnancy. ACOG Committee Opinion No. 299. Obstet Gynecol 2004 (Reaffirmed 2014)104:647-51.
7. Revel MP, Sanchez O, Couchon S, et al: Diagnostic accuracy of magnetic resonance imaging for an acute pulmonary embolism: results of the “IRM-EP” study. J Thromb Haemost 2012;10:743-750.
8. Rajaram S, Exley CE, Fairlie F, Matthews S: Effect of antenatal iodinated contrast agent on neonatal thyroid function. Br J Radiol 2012, 85:238-242.
9. Stein PD, Chenevert TL, Fowler SE, et al: Gadolinium-enhanced magnetic resonance angiography for pulmonary embolism: a multicenter prospective study (PIOPED III). Ann Intern Med 2010;152:434-443.
10. Kalb B, Sharma P, Tigges S, Ray GL, Kitajima HD, Costello JR, Chen Z, Martin DR: MR Imaging of Pulmonary Embolism: Diagnostic Accuracy of Contrast-enhanced 3D MR Pulmonary Angiography, Contrast-enhanced Low–Flip Angle 3D GRE, and Nonenhanced Free-Induction FISP Sequences. Radiology 2012;263:271-278.
11. Mudge CS, Healy TT, Atalay MK, Pezzullo JA: Feasibility of Detecting Pulmonary Embolism Using Noncontrast MRI. ISRN Radiology 2013 (2013), ID 729271, 5 pages.
12. Moradi M: Pulmonary thromboembolism in pregnancy: Diagnostic imaging and related consideration. J Res Med Sci 2013;18:255-259.
13. B Hochhegger B, Ley-Zaporozhan J, Marchiori E, Irion K, Soares-Souza A, Moreira J, Kauczor HU, Ley S: Magnetic resonance imaging findings in acute pulmonary embolism. Br J Radiol 2011;84:282-287.







